All, Announcements
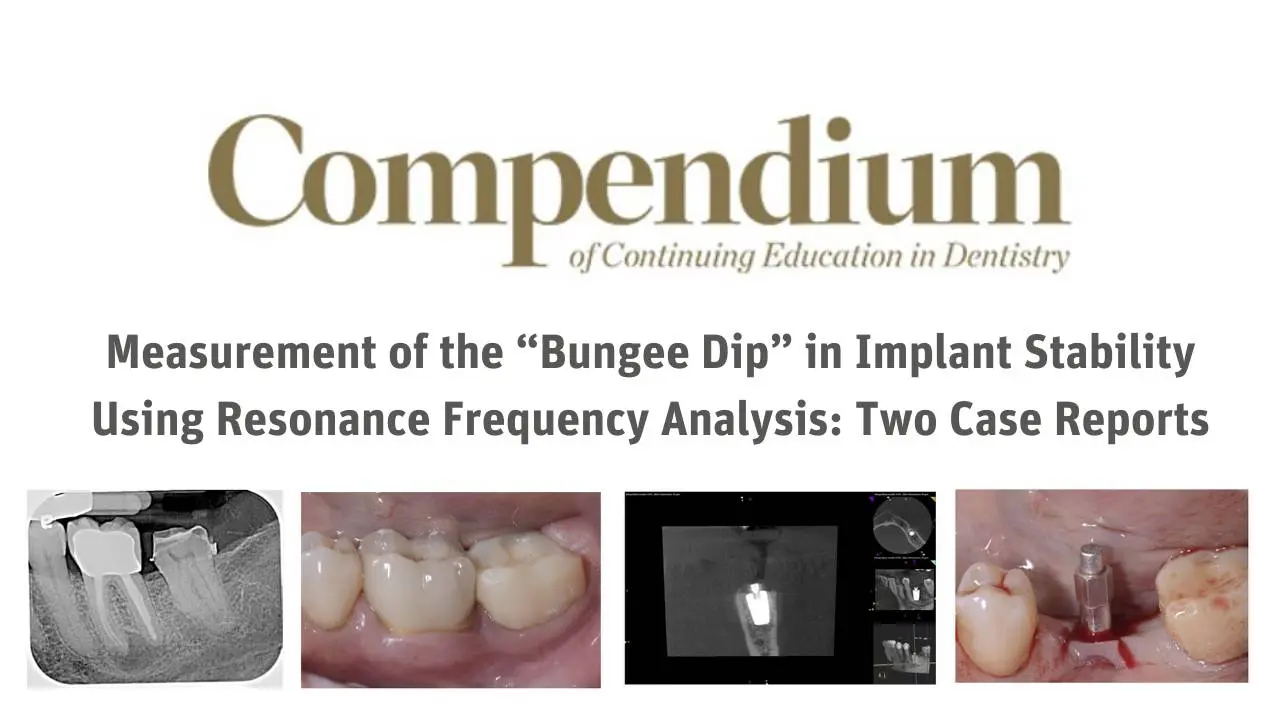
Measurement of the “Bungee Dip” in Implant Stability Using Resonance Frequency Analysis: Two Case Reports
About the Author
Dr. Paul Rosen has maintained a full-time private practice in Lower Bucks County for over 25 years limited to periodontics, surgical implant placement and regenerative therapy. He also has academic appointments as Clinical Professor of Periodontics at the University of Maryland Dental School and Clinical Professor of Periodontics and Oral Implantology at Temple University Dental School. Dr. Rosen is board certified (Diplomate of the American Board of Periodontology) where he also has been an examiner. Dr. Rosen is a Fellow of the American College of Dentists and is known throughout the United States and internationally having written over 50 articles and 5 book chapters.
He continues to be involved in research and his lectures have advanced periodontal and dental implant treatment, focusing on cutting edge techniques and innovative products. Dr. Rosen has been recognized by his peers in Philadelphia Magazine as one of the top dentists in the region and in 2015, Dr. Rosen received the Master Clinician Award, by the American Academy of Periodontology which is conferred to only one member annually who has demonstrated consistent clinical excellence in periodontology. The Master Clinician Award is considered one of the American Academy of Periodontology’s highest honors.
Abstract: Implant stability is a key consideration when determining the point in time a dental implant should be loaded. Often a change in implant stability is observed as healing progresses from initial mechanical stability to biologic stability, ie, osseointegration, during the bone modeling/remodeling process. This change in stability can be objectively measured using resonance frequency analysis (RFA). Because bone healing varies from patient to patient, the timing of this sequence may be unpredictable; in a small subset of patients the drop in implant stability can be quite precipitous and profound. Such a drop is referred to as a “bungee dip.” If the implant is loaded too prematurely, it may fail due to inadequate healing. This article presents two case reports that demonstrate the use of RFA and its values, known as implant stability quotients, to monitor implant stability during healing. RFA is a form of personalized care that provides objective evidence that can guide the clinician in establishing safe and successful loading protocols.
Case Preview:
Case 1: Mandibular First Molar
A 63-year-old female patient in good general health was referred for evaluation and placement of an implant at the site of a failing mandibular left first molar. The tooth previously had undergone endodontic treatment more than a decade prior but had recently become symptomatic. Clinical and radiographic examination of the area revealed no mobility of the teeth, probing depths ranging from 1 mm to 3 mm (Figure 1), and a large radiolucent lesion at the mesial root of the mandibular left first molar (Figure 2). Based on these considerations and consultation with an endodontist, the prognosis for this tooth was questionable to hopeless.
Case 2: Maxillary Second Molar
A 54-year-old female patient in good general health was referred for evaluation and placement of an implant at the site of a missing maxillary left second molar (Figure 11). Pretreatment assessment determined that adequate bone was available in both the buccal-palatal and vertical dimensions for implant placement without the need for any additional procedures.
Following reflection of a full-thickness flap, the implant osteotomy was prepared and a 4.5 mm diameter x 9 mm length tapered dental implant with an electrowetted surface (ProActive®) was placed into type 2 bone. The final seating torque of 35 Ncm and ISQ values of 71 and 70 (Osstell IDx) in the buccal-palatal and mesial-distal directions, respectively, confirmed adequate primary stability before flap closure (Figure 12). A PEEK healing abutment was placed (Figure 13) prior to flap suturing, and the implant was allowed to heal transgingivally.


Comments are closed.