Ceramic implants are one of the relatively newer and most exciting developments in oral implantology. These implants have been used in Europe since the early 2000s and, subsequent to FDA approval in 2011, in the United States. The first ceramic material that was used in the past for dental implants was aluminum oxide. This material showed good osseointegration, but it did not have adequate mechanical properties for long-term loading. More recently, a new generation of ceramic materials, such as zirconia (ZrO2), was introduced.
Zirconia is characterized by more favorable mechanical properties than aluminum oxide: higher flexural strength (900 to 1,200 MPa), hardness (1,200 Vickers), and Weibull modulus (10 to 12).1 This material also demonstrates high biocompatibility2 and low plaque adhesion.3 Several animal studies have shown bone-to-implant contact similar to titanium.4 The use of advanced nanotechnology for implant surface modification to improve the osseointegration process of ceramic implants has also been reported.5

Primary biological considerations for ceramic implants are improved gingival health and lower rates of peri-implantitis. This can be attributed to lower plaque accumulation around ceramic implants and no release of titanium ions, as well as a shift to a healthier microbiome.6
Titanium implants, in contrast, after interacting with intraoral conditions, undergo tribocorrosion and release titanium particles into the surrounding gingivae.7 This release of ions can contribute to the subsequent inflammation around titanium dental implants.8 Zirconia, in contrast, is bio-inert and does not react with the oral environment. Recent literature has shown that zirconia implants induce little to no peri-implant tissue inflammation and allow for improved levels of epithelial attachment.9
Another major advantage of zirconia implants is the improved aesthetics, especially in cases of thin bone or thin gingival biotypes. In these cases, with titanium implants, a dark shadow is usually visible around the gumline. This issue is resolved with zirconia implants, which are opaque white in shade and have a neutral effect on the gingival tone. The peri-implant soft tissue around zirconia demonstrated a better color match to the soft tissue at natural teeth than titanium.10
Indications for metal-free zirconia dental implants are multifold and can be divided into 2 categories: biological and patient demand. From a biological standpoint, metal allergies are one of the main reasons to use these implants. Research has shown that 0.6% of the population has hypersensitivity-type reactions to titanium.11 What is more, in patients who have had reactions to metals in dental materials, the allergy symptoms were resolved after the implants or devices were removed.12
Patient demand has been the major driving force behind finding and adopting metal-free tooth replacement solutions. A recent survey conducted in Europe showed that 65% of the patients would prefer a metal-free implant.13
When it comes to the clinical outcomes of ceramic implants, a recent systematic review and meta-analysis showed that zirconia implants present a survival rate of 91.5% to 98.3%, a success rate of 91.6%, and marginal bone loss ranging from 0.7 to 0.98 mm.14
This article presents 2 cases that demonstrate using zirconia dental implants to replace a missing natural tooth in areas of high aesthetic demand.
CASE REPORTS
Case 1: Anterior Immediate Implant

Figure 1. Periapical radiograph of the lateral incisor showing failed endodontic treatment and a defective restoration.
Replacement options were discussed, and the patient chose a fixed replacement solution with a metal-free dental implant. Some reasons for this decision were the health of peri-implant tissues around ceramic implants and the desire for a metal-free solution.
In consideration of local and systemic factors, extraction and immediate placement of the implant was recommended. Local anesthesia was administered by infiltration on buccal and palatal sides, and the remaining root was atraumatically extracted using periotomes and forceps. An implant osteotomy was done using copious irrigation and manufacturer protocols, and a 3.5- × 10-mm Zeramex XT implant (Dentalpoint AG) was placed (Figure 2).
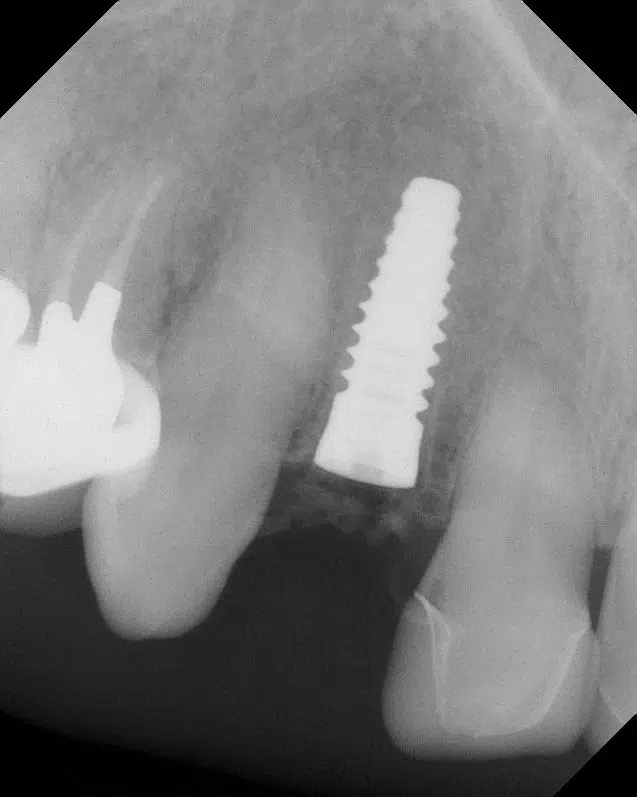
Figure 2. A Zeramex XT 3.5- × 10-mm zirconia implant (Dentalpoint AG) placed immediately after the extraction.
The final torque of implant placement was 35 N/cm2; implant stability quotient (ISQ) values of 67 were measured using the Ostell Beacon device (W&H Dentalwerk). Phlebotomy was done to create PRF membranes and sticky bone in order to graft the remainder of the socket and initiate the regenerative protocol. A healing abutment was placed onto the implant, and an Essix-type appliance was fabricated to be worn during the healing phase.
Four months after the extraction and immediate placement, the patient returned for the restorative phase. Clinical examination showed healthy soft tissues around the implant with an abundance of keratinized gingiva (Figure 3). A closed-tray impression coping was used for the final impression (Figure 4).

Figure 3. Soft-tissue contours and healing 4 months after the surgery.

Figure 4. A closed-tray impression coping is used to take the final impression for the restoration.
A bite registration and photographs were also used for the fabrication of the final prosthesis. The customized zirconia abutment (Figure 5) was attached to the implant, and a porcelain-layered zirconia crown was cemented in place (Figure 6). Radiographs were used to confirm the seat of both the abutment and crown and the complete removal of cement (Figure 7).

Figure 5. A customized zirconia abutment with the laboratory screw is shown

Figure 6. The final restoration is delivered, showing good pink and white aesthetics and a natural fit.

Figure 7. The final periapical radiograph of the implant and the restoration.
Case 2: Premolar Delayed Implant
A 38-year-old healthy female patient presented to us with an edentulous space at the tooth No. 13 site; the tooth had been fractured and extracted one year prior. Clinical and radiographic evaluation demonstrated adequate bone volume and adequate soft-tissue quality and quantity (Figure 8).

Figure 8. A preoperative photograph of the proposed implant site No. 13, showing adequate hard- and soft-tissue volume.
A straightforward implant placement was planned after discussing the options, and a 4.1- × 10-mm Straumann Pure 2-piece Ceramic Implant System (Straumann) was inserted using manufacturer protocols (Figure 9). The final insertion torque was 40 N/cm2, and ISQ values of 83 were obtained.
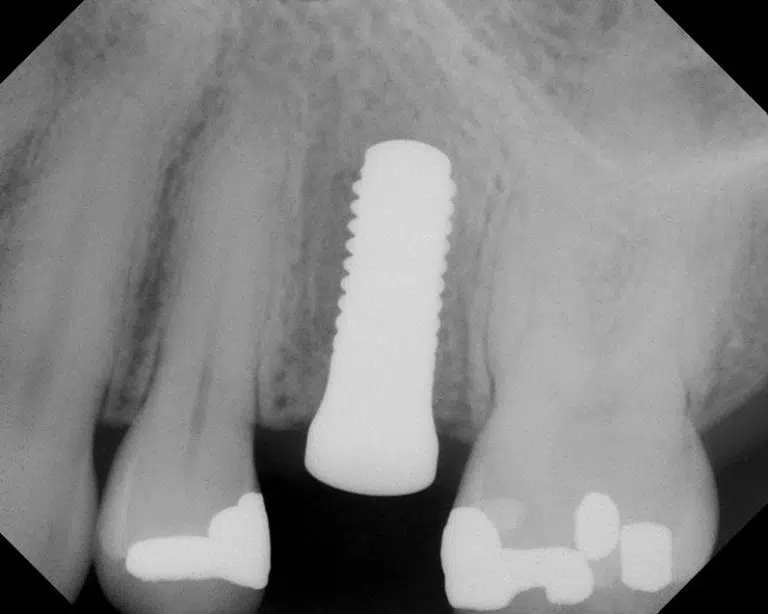
Figure 9. A periapical radiograph of the 4.1- × 10-mm Straumann Pure Ceramic Implant System (Straumann) on the day of surgical placement.
A ceramic healing abutment was placed, and the surgery site was closed using 4.0 chromic gut sutures (Figure 10).

Figure 10. A zirconia healing abutment was placed at the time of insertion, and the flaps were approximated using 4.0 chromic gut sutures.
Prosthetic steps were initiated 12 weeks after the healing process. Figure 11 shows the excellent health of gingival tissues around the implant and the abundance of attached keratinized tissues vertically and horizontally. A scanbody was used to digitally capture the implant position, adjacent structures, and soft-tissue emergence profile.

Figure 11. Soft-tissue contours and health after 3 months of healing.
The final screw-retained restoration (Figure 12) was produced and delivered using standard protocols. The seating of the restoration was confirmed by a bite-wing radiograph (Figure 13). The patient’s new implant restoration blended in well with her existing teeth, gums, and oral harmony (Figure 14).

Figure 12. The final screw-retained ceramic restoration is shown.
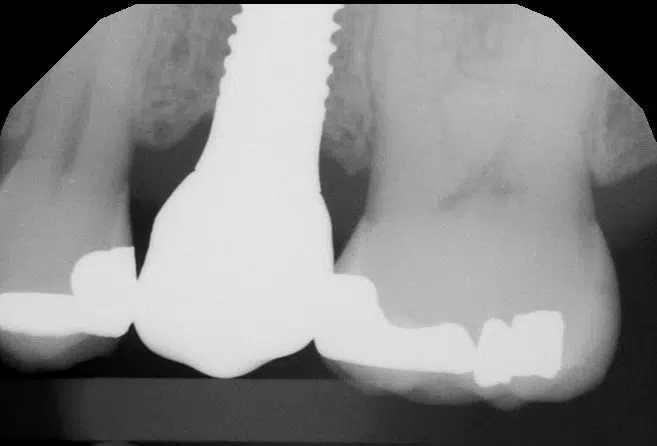
Figure 13. A bite-wing radiograph confirming the complete seat of the restoration is pictured.

Figure 14. The ceramic implant and the ceramic restoration blend harmoniously with the patient’s existing dentition, restoring function and aesthetics.
DISCUSSION
Ceramic implants are gaining popularity worldwide as an excellent option for tooth replacement. As the demand for metal-free solutions increases, more research is being done in the field of zirconia implant materials, surface characteristics, and implant designs. Many studies have investigated the behavior of zirconia dental implants on hard and soft tissues and have found very favorable outcomes that match and, in certain parameters, exceed that of titanium implants.15
The rising incidence of peri-implant mucositis and peri-implantitis affects both the short- and long-term survival rates of titanium implants and their success. Therefore, using an alternative material, zirconium dioxide, has been increasingly popular and successful. Zirconia has been shown to have similar integration success compared to titanium, offers a soft-tissue response that is superior to that of titanium, and has less affinity to collect plaque or biofilm compared with titanium surfaces.
In addition to this, scientific advances have allowed the creation of modified zirconia implant surfaces to improve and accelerate bone healing response and clinically reduce the healing time. Recent bioengineering studies have shown that zirconia can be set into a bioactive system by embedding diverse bio-molecules into the structure of the implant. This allows for a more realistic display of bone tissue structure at a macro and micro molecular level and induces cell responses that improve the treatment outcomes with zirconia implants.16
The characteristics of their enhanced biocompatibility, along with good osseointegration and success rates, make zirconia implants clear candidates for use in clinical implant dentistry.17
CONCLUSION
In areas of aesthetic demand, where soft-tissue complications can have a more obvious and immediate impact, zirconia dental implants may offer both surgical and restorative clinicians an excellent level of security and flexibility.
Read the full article by CLICKING HERE

Comments are closed.