All, Whole Body Health
Solving Ceramic Crown Removal and Endo Access Challenges
INTRODUCTION
Clinically, a tooth with a fixed restoration may need to undergo endodontic treatment or require replacement of the crown. There are a host of reasons for the removal of existing fixed restorations, which include replacement of the crown related to recurrent decay, replacement following endodontics, fracture of the existing restoration, or conversion to a fixed abutment for a bridge. There may also be situations where existing crowns will be maintained but endodontics must be performed on those teeth as well, requiring the preservation of the current restorations.
Various materials have been utilized for fixed restorations: some metal-based and others ceramic metal or all ceramic in nature. Starting about 3 decades ago, the direction has been to place far fewer metal-free fixed restorations due to the increasing demand from patients for more aesthetic restorations. Underlying this move is that we have witnessed the introduction of new, stronger, and more aesthetic ceramic dental materials. Ceramics, whether they are feldspathic, leucite reinforced, or lithium disilicate-based, are fairly easy to cut through when needing to access the pulp chamber to perform endodontic procedures or remove the existing crown for replacement. In the last decade, we have seen many laboratories and doctors moving toward the use of both layered and monolithic zirconia restorations. This very strong and tough material has come with increased frustration to the practitioner when these restorations need to be removed or if endodontic access is required through the restoration. Of course, as with any procedure, the selection of the correct instruments and techniques will improve the performance and outcomes while decreasing the time to achieve the desired results and eliminating operator frustration. In this article, methods to access through and remove zirconia-based restorations will be discussed. Additionally, techniques for metal-based restorations will be addressed.
Ceramic Materials Differ
Zirconia hardness, as measured by the Vickers hardness number (VHN), is reported in the range of 700 to over 1,200, depending on how the material is treated during manufacturing and how it is fired following milling.1 The hardness of zirconia restorations can decrease over time with acidic drinks (ie, colas and citrus juices), but this affects non-zirconia-based ceramics to a greater extent.2 Flexural strength also is greater for monolithic zirconia restorative materials, decreasing for zirconia hybrid ceramics and further for lithium disilicate and leucite-reinforced ceramics.3 These properties correlate with the abrasiveness of the restorative material.4
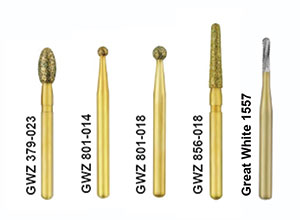
Figure 1. Great White Zirconia (GWZ) diamonds (SS White) that are utilized for zirconia crown removal or endodontic access. The metal carbide is for use on all-metal crowns or the metal base of PFM restorations.


Figure 2. The diamond is held against the buccal surface of the
crown with light pressure and moved in a direction that is
parallel to the long axis of the diamond to create a slot through
the ceramic.
Figure 3. The diamond continues to be used in a direction |


Figure 4. A slot is next cut across the occlusal surface in a similar manner that is continuous with the slot cut on the buccal surface, again moving the diamond parallel to the long axis of the diamond.


Figure 6. A flat-bladed instrument tip is inserted in the buccal groove and rotated from left to right to create torque to split the crown at the slots.
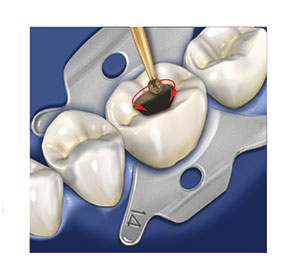

Figure 8. Once the crown material has been penetrated to the dentin in the outline form, access through the crown is completed.
Zirconia Crown Removal
The key to removal of a zirconia crown is creating a slot across the buccal and occlusal/incisal so that an appropriate torqueing force can be applied to split the crown while preserving the underlying tooth structure. Of course, it is important to be aware that excessive force can cause a cohesive tooth fracture depending on the cementation method used, the tooth size, and the resulting luted tooth-to-restoration surface area present. So one must apply a prudent and safe level of force, realizing that additional slots may be advisable, or, in some cases, the restoration may even need to be prepped off the tooth, section by section.
For this protocol, a medium-grit, slightly tapered diamond (Great White Zirconia 856-018 [SS White]) (Figure 1) is used in a high-speed handpiece with copious water and light pressure against the tooth and is moved parallel to the diamond’s long axis in a “sawing” motion (Figure 2). This starts on the mid-buccal surface to create a slot from the crown margin to the junction with the occlusal or incisal surface (depending on which tooth is being treated). The slot is periodically checked to avoid penetration into the underlying dentin (Figure 3). With a posterior crown, once the slot has fully penetrated through the zirconia, an additional slot is cut across the occlusal surface that is continuous with the buccal slot (Figure 4). When the crown being removed is on an anterior tooth, the incisal of the crown requires a slot deep enough to reach the underlying dentin (Figure 5). As the crown may be fairly thick in this area, depending on how the original tooth was prepared or what remained of the tooth prior to preparation, this slot may be up to 3.0 mm deep or more. A flat-bladed instrument, such as a crown remover or an enamel hatchet, is inserted into the buccal slot where it continues with the occlusal/incisal slot. Then a rotational torqueing motion is made to split the restoration into 2 halves, thus separating it from the prepared tooth (Figure 6). It is not advisable to attempt this with a flat-bladed composite instrument as the torque generated will either break the tip of the instrument or deform it. Crown removal instruments are preferred because they are better designed to withstand the forces generated without instrument breakage. Should the crown not split into 2 pieces, verify that both grooves are continuous to the dentin, and deepen them if ceramic remains in the slots. If the slots have penetrated to the dentin and the crown is not splitting, then continue the slot 2.0 to 3.0 mm onto the lingual surface. Should that still not allow crown splitting, then, using the same diamond, remove ceramic interproximally (at the expense of the crown being removed) to create space to allow the crown halves to separate when torqued with the instrument.
Dental adhesives are less retentive to zirconia than tooth structure, and there is a debate on whether or not a true adhesive bond occurs to this substrate.5 Upon crown removal, the luting material often remains bonded to the dentin, and this can be taken off during re-preparation of the tooth. This also pertains to layered zirconia restorations that have an overlying porcelain layer that was applied for improved aesthetics. On the other hand, ceramics such as lithium disilicate ceramics, leucite-reinforced ceramics, and other all-ceramics (including those containing zirconia particles as well as ceramic resin hybrids) have true adhesion between the crown material and tooth structure.6-8 These may not split with the 2 slots created or the removal of interproximal crown material. The author has found this to be more frequent in the posterior. When this is encountered, creating an additional slot from mesial to distal that includes the marginal ridges (creating a plus-shaped slot across the occlusal) with placement of the crown splitter instrument into the mesial slot and applying rotational torque separates either the MB or ML cusp portion of the crown from the tooth. This is repeated in the distal slot, then, depending if the buccal or lingual crown material remains, the instrument is placed into the remaining slot. This technique will usually loosen the remaining crown material.


Figure 10. Unroofing the pulp chamber may be accomplished with the diamond or a carbide bur (practitioner preference), and then the endodontic access is completed.
Figure 11. The diamond is used to create the slot in the |


Figure 12. The carbide is utilized to continue the slot through the metal to the underlying dentin.

Figure 14. Following outline form with the round diamond to the underlying metal substructure of the crown, the carbide is utilized to complete endodontic access to unroof the pulp chamber.
Endodontic Access Openings Through Zirconia
A medium-grit round diamond is used for this procedure. The round diamond is provided in 3 sizes, and selection is based on what tooth is being treated and the size of the access form needed for endodontic treatment. Lower anterior teeth and maxillary lateral incisors will have smaller endodontic accesses and will utilize a GWZ 801-014 bur (SS White) (Figure 1). Maxillary central incisors and canines, as well as both maxillary and mandibular premolars, will require a larger access to unroof the pulp chamber, and a GWZ 801-018 bur (SS White) (Figure 1) is best suited for these teeth. The round medium diamond is again used with light pressure, constant motion, and copious water (Figure 7). The diamond is used to outline the access form desired and not pressed/pushed into the ceramic crown material in an attempt to create a hole through the restoration (Figure 8). Molars require the largest endodontic accesses due to the dimensions of their pulp chambers, and the widening of the initial access opening through the ceramic crown using the GWZ 801-018 can be followed with a football-shaped GWZ 379-023 bur (SS White) (Figure 1) to achieve the desired access shape. A carbide bur is utilized to unroof the pulp chamber (Figure 9). Once the pulp chamber has been penetrated, the outline form may also be refined using the GWZ 856-018; then endodontic treatment of the canal system can begin (Figure 10).
All-Metal or Porcelain-Fused-to-Metal (PFM) Restorations
As discussed, metal cannot be as efficiently cut with a diamond, and a carbide bur is, thus, the preferred option. When crown removal is planned, the GWZ 856-018 diamond is utilized to create the slots through the ceramic layer until the metal substructure is encountered (Figure 11). A Great White #1557 metal-cutting carbide (SS White) is then applied at the buccal margin and stroked in an occlusal direction with the rotary instrument tip penetrating to the dentin and continuing to the occlusal/incisal surface (Figure 12). Once the slot has been completed to the dentin, the crown removal instrument is placed into the groove and torqued to complete the removal of the crown. The process is similar with all-metal crowns, eliminating use of the diamond and being completed with the carbide bur alone (Figure 13).
Endodontic access is also approached in a similar manner as when dealing with all-ceramic crown materials. When a PFM restoration requires access though the restorative material for an endo procedure, one of the round diamonds (GWZ 801-014 or GWZ 801-018) is used to create an outline form slightly larger than needed through the ceramic to the underlying metal. The Great White #1557 carbide is then used to form a hole through the metal into the dentin. Then the outline form is widened to the dimensions of the outline created in the ceramics with the carbide and through the dentin to unroof the pulp chamber (Figure 14).
Typically, access in precious and semi-precious metals can be performed with a single carbide, but non-precious metals may require multiple carbides to complete the task. This also is true with restoration removal of PFM crowns. All-metal crowns require more metal to be removed and usually require multiple carbide burs to accomplish the task. Using light pressure allows the carbide to cut metal more efficiently and is less likely to snap the head off the bur, which may occur when excessive pressure is applied to the restoration. The carbide should be disposed of after a single crown removal or endodontic access or if, during the procedure, it stops cutting the metal. The diamonds may be used several times and should be discarded when the diamond particles begin to fall off the shaft of the rotary instrument. This can be typically noted by baldness on the tip as that area takes the most stress when in use.
CLOSING COMMENTS
Crown removal and endodontic access can be accomplished with efficiency and decreased chair time when the diamond and carbide burs mentioned herein are utilized as described. Light pressure with a stroking motion (for crown removal slot preparation) or circular outline formation (for endodontic access) with copious irrigation improves efficiency while decreasing stress on the rotary instrument as well as the practitioner.
Acknowledgment:
The author would like to thank Robert Wojciechowski for the illustrations in this article.
About the Author

Dr. Gregori M. Kurtzman, DDS, MAGD, DICOI, DIADI
He is in private general practice in Silver Spring, Md. A former assistant clinical professor at the University of Maryland, he has earned Fellowships in the AGD, the American Academy of Implant Prosthodontics, the American College of Dentists, the International Congress of Oral Implantologists (ICOI), the Pierre Fauchard Academy, and the Association of Dental Implantology; Masterships in the AGD and ICOI; and Diplomate status in the ICOI and the American Dental Implant Association. He has lectured internationally, and his articles have been published worldwide. He has been listed as one of Dentistry Today’s Leaders in Continuing Education since 2006. He can be reached via email at [email protected].
Reference: https://www.dentistrytoday.com/articles/10713

Comments are closed.