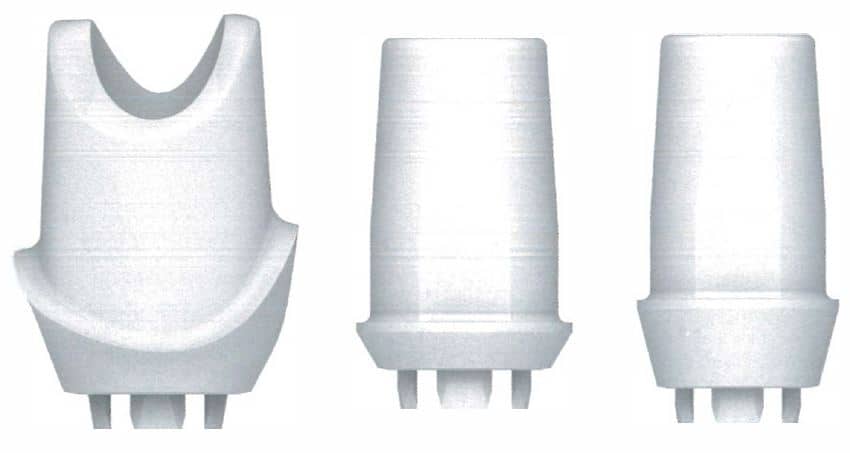
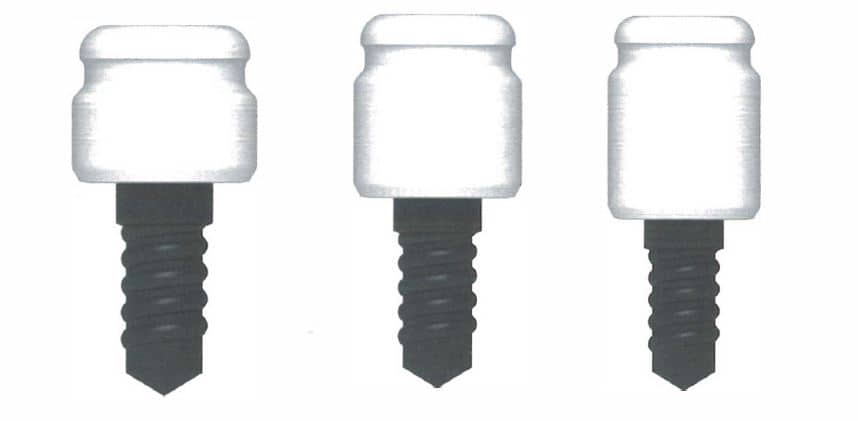
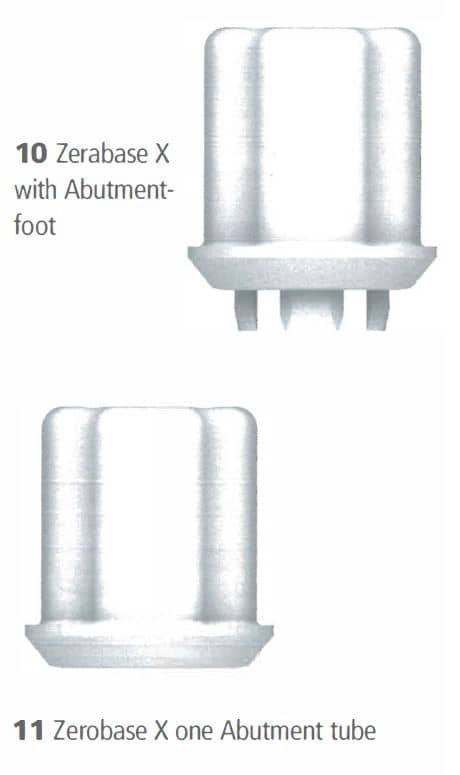
The post ZERAMEX launches further innovations in dental implantology appeared first on Emerginnova.
]]>The post ZERAMEX launches further innovations in dental implantology appeared first on Emerginnova.
]]>The post ZERAMEX as a featured product by Klaus Pettinger and Wolfgang Weisser appeared first on Emerginnova.
]]>The post ZERAMEX as a featured product by Klaus Pettinger and Wolfgang Weisser appeared first on Emerginnova.
]]>A: I've always said, "Don't use the bumper sticker that reads floss or die." In other words, we need to stop telling patients that if they don't see us, they're going to die of heart disease. No, you're only going to die of heart disease maybe earlier if you already are genetically susceptible to periodontitis and other chronic inflammatory diseases.
As dental professionals, we have to have the correct perspective. If we're not careful about the oral-systemic link, people are going to think we're crying wolf. This isn't about just talking about the oral-systemic link, but rather personalizing it for each patient. It is taking into consideration the patient's medical history and dental history and matching the two together.
I think so often dental practices cookie cut when explaining the oral-systemic link. You must boil it down so it is simple and meaningful for that patient in your chair. Link it to that patient and his or her medical history, including familial history.
Here's an example. This is the way I've always dealt with the smoking issue among my patients. My parents were smokers, so I have a history there.
How do you handle patients who smoke because you know there's a great link between nicotine and periodontal disease? Here's what I say: "You know your chances of losing your teeth are five times greater if you smoke. I'm OK if you want to continue smoking. That's up to you. I'm just suggesting to you that it's going to be a five times greater risk. I'm not going to harass you about it, but you're the one who has to make that decision, not me. And we will modify that we need to see you more often and your home care must be better than average."
Q: So if someone has really never jumped into the oral-systemic link and wants some research to share with those patients who might be affected, what do you suggest?
A: The American Academy of Periodontology still is the best resource. And for studies, refer to the American Journal of Cardiology when it comes to heart disease. I would start with this paper from Friedewald et al.
Q: Any final thoughts?
A: We dentists, on occasion, still think we are "dentists," but we don't realize that we're actually oral physicians and oral healthcare professionals. Until we see the mouth as an organ and just as important as any other organ, it's going to be really difficult to truly impact the lives of our patients in a more meaningful way. However, there is still hope.
The comments and observations expressed herein do not necessarily reflect the opinions of DrBicuspid.com, nor should they be construed as an endorsement or admonishment of any particular idea, vendor, or organization.
The post Q&A with Dr. Sam Low on COVID-19 and inflammation, plus personalizing the oral-systemic link appeared first on Emerginnova.
]]>The post Q&A with Dr. Sam Low on COVID-19 and inflammation, plus personalizing the oral-systemic link appeared first on Emerginnova.
]]>The post The mouth-gut axis: How poor oral health may worsen gut inflammation appeared first on Emerginnova.
]]>The post The mouth-gut axis: How poor oral health may worsen gut inflammation appeared first on Emerginnova.
]]>The post “I am convinced that the use of ceramic implants will constantly grow in the future” appeared first on Emerginnova.
]]>The post “I am convinced that the use of ceramic implants will constantly grow in the future” appeared first on Emerginnova.
]]>The post Straumann asks, “Will ceramics soon become the new material of choice” appeared first on Emerginnova.
]]>The post Straumann asks, “Will ceramics soon become the new material of choice” appeared first on Emerginnova.
]]>The post Titanium Corrosion in the Oral Environment appeared first on Emerginnova.
]]>The post Titanium Corrosion in the Oral Environment appeared first on Emerginnova.
]]>The post Oral cancer diagnoses in the U.K. increased 50% in 10 years appeared first on Emerginnova.
]]>The post Oral cancer diagnoses in the U.K. increased 50% in 10 years appeared first on Emerginnova.
]]>The post Oral health plays an increasing role in overall health during aging appeared first on Emerginnova.
]]>The post Oral health plays an increasing role in overall health during aging appeared first on Emerginnova.
]]>The post How to start talking to patients about the oral-systemic connection appeared first on Emerginnova.
]]>The post How to start talking to patients about the oral-systemic connection appeared first on Emerginnova.
]]>





 Stefan Röhling
Stefan Röhling


